
Fil d'Ariane
- Nouvelles et événements
- Nouvelles
- Content
- Une toute première thérapie efficace pour des maladies neurodégénératives rares et dévastatrices
null Une toute première thérapie efficace pour des maladies neurodégénératives rares et dévastatrices
Avec le soutien d'une organisation à but non lucratif créée par la famille d'un patient, le Dr Kenneth Myers, spécialiste des maladies rares, a lancé un essai clinique pour un traitement prometteur d'une maladie grave et mortelle causée par des mutations du gène POLG. Les résultats dépassent toutes les attentes.
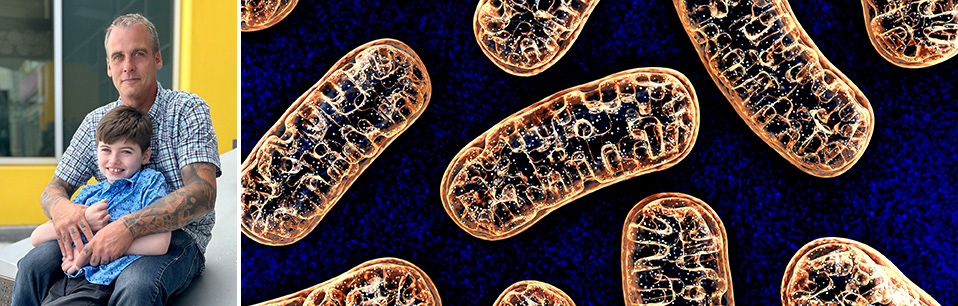
Montréal, le 29 juillet 2024— Un nouveau traitement pourrait améliorer la vie des patients atteints de maladies mitochondriales appelées maladies liées au gène POLG, selon un essai clinique unique mené à l'Institut de recherche du Centre universitaire de santé McGill (IR-CUSM). Les patients atteints de ces maladies présentent un déclin neurologique progressif et ont une survie médiane de cinq mois après l'apparition des symptômes. Les résultats préliminaires de l'essai clinique ouvert de phase 2, publiés dans la revue eClinicalMedicine, ont montré que la thérapie combinée désoxycytidine/désoxythymidine est un traitement sûr et potentiellement efficace pour les maladies liées au gène POLG. L'étude a été presque entièrement financée par la Fondation Liam, qui porte le nom d'un patient diagnostiqué en 2019 d'un trouble lié au gène POLG à l'Hôpital de Montréal pour enfants (HME).
« Notre étude donne un nouvel espoir aux familles touchées dans le monde entier, car le diagnostic d'un trouble lié au gène POLG implique une régression du développement moteur et cognitif de l'enfant et constituait auparavant une sentence de mort, dit le Dr Kenneth Myers, neurologue pédiatrique à l'HME et scientifique au sein du programme en santé de l'enfant et en développement humain à l’IR-CUSM. Le traitement étudié ne guérit pas, mais l'état clinique des patients de notre cohorte est bien meilleur que ce à quoi on aurait pu s'attendre, sachant que la mort survient souvent quelques mois seulement après l'apparition des symptômes. Les patients de notre cohorte ne sont pas seulement en vie, ils se portent mieux. »
Réparer les centrales énergétiques de l'organisme
Les maladies mitochondriales sont caractérisées par un dysfonctionnement des mitochondries, les structures cellulaires qui produisent l'énergie dont les cellules humaines ont besoin pour fonctionner normalement. Dans le monde, on estime qu'une personne sur 5 000 est atteinte d'une maladie mitochondriale génétique.
Dans les maladies liées au gène POLG, les mutations affectant ce gène entraînent une réduction de la teneur en ADN mitochondrial (ADNmt), qui est essentiel au fonctionnement normal des mitochondries. Il en résulte une série de signes et de symptômes pouvant inclure des crises d'épilepsie, une perte de vision, un dysfonctionnement musculaire (myopathie), des lésions nerveuses (neuropathie), des troubles du développement ou une régression, ainsi qu'une insuffisance hépatique. Le traitement mis à l’essai par le Dr Myers, qui a déjà été utilisé pour une autre maladie mitochondriale, cible le mécanisme génétique défectueux qui entraîne l'appauvrissement de l'ADN mitochondrial.
Après six mois de traitement, les scores des patients sur la Newcastle Mitochondrial Disease Scale - une échelle clinique validée utilisée pour évaluer la progression de la maladie mitochondriale - étaient plus bas, ce qui suggère une efficacité de la thérapie à l’essai. Les chercheurs signalent également une diminution des taux sériques du facteur de croissance et de différenciation 15 (GDF-15), un biomarqueur quantitatif du dysfonctionnement mitochondrial. Enfin, les proches aidants des patients ont fait état d'une amélioration clinique, notamment en ce qui a trait au niveau d'énergie, à la fonction motrice, à l'état cognitif et à la communication. Aucun événement indésirable grave attribuable au traitement n'a été signalé.
« De nombreux patients participant à l'étude se portaient bien et se développaient tout à fait normalement jusqu'à ce qu'ils contractent une infection ou qu'un autre évènement ne déclenche la maladie POLG et qu'ils régressent complètement, perdant leur capacité à marcher, à parler ou à s'alimenter. C'est une véritable tragédie pour la famille lorsque cela se produit, explique le Dr Myers. Avec ce médicament, nous donnons aux patients les éléments constitutifs de l'ADN mitochondrial qui leur manquent, afin d'aider leurs mitochondries à produire l'énergie dont leurs cellules ont besoin pour fonctionner correctement. »
« Une patiente était asymptomatique jusqu'à l'âge de 15 ans, quand son état a commencé à se détériorer. Elle a commencé à avoir des crises d'épilepsie et à souffrir de faiblesse et de problèmes d'équilibre, de sorte qu'elle ne pouvait plus faire que quelques pas toute seule. Depuis qu'elle a commencé l'essai, elle n'utilise plus de fauteuil roulant et mène essentiellement la vie d'une adolescente normale », ajoute le Dr Myers.
La nouvelle publication rapporte les résultats des dix premiers enfants et adolescents atteints de mutations POLG recrutés pour l'essai, dont certains sont venus des États-Unis, du Brésil et de l'Inde pour y participer. Tous ont reçu le même traitement, la désoxycytidine/
désoxythymidine, prise par voie orale trois fois par jour, pendant une période initiale de six mois. La période de traitement a été prolongée à 24 mois après que certains participants eurent obtenu des réponses positives significatives et souhaité poursuivre la thérapie. Depuis, 14 patients supplémentaires ont participé à l'essai, et une publication décrivant les effets à long terme de la thérapie sur un groupe plus grand de patients est en cours de préparation.
L'histoire de Liam : Quand la vie prend un tournant
Liam est un enfant de dix ans atteint d'une maladie mitochondriale causée par des mutations du gène POLG.
En mai 2019, Liam a commencé à avoir des crises d'épilepsie et a été amené à l'HME. Il y est resté environ cinq semaines, faisant des crises presque 24 heures sur 24 jusqu'à ce qu'il obtienne le bon assortiment de médicaments. Lorsqu'il est rentré chez lui, il avait perdu toute capacité de communication. Peu après, en juin 2019, il a commencé à avoir de nouvelles crises et a été réadmis à l'hôpital. C'est alors que les résultats des tests génétiques sont arrivés et que le diagnostic de POLG a été posé.
« Lorsque Liam a été diagnostiqué, on nous a dit que son état s'aggraverait avec le temps et qu'il perdrait la vie à cause de cette maladie. Cette nouvelle a bouleversé notre famille et a changé le cours de ma vie », confie le père de Liam, Kevin Reason, qui depuis se dévoue à la cause.
Le Dr Myers lui a parlé de la désoxycytidine/désoxythymidine, un nouveau traitement susceptible d'aider Liam, et ils ont décidé ensemble de lancer un essai clinique. Kevin a créé la Fondation Liam pour le financer.
« Aujourd'hui, Liam est capable de marcher à nouveau, de communiquer et de sourire. Tout ce que nous voyons, c'est une amélioration, dit Kevin. Nous savons que ce traitement n'est pas curatif, mais il nous donne de l'espoir. Et il nous fait gagner du temps précieux, le temps dont nous avons besoin pour trouver une façon de guérir la maladie. »
Liam a été le premier patient atteint d'une maladie liée au gène POLG à essayer le traitement en Amérique du Nord. Grâce à la Fondation Liam et au soutien d'autres organisations à but non lucratif, 23 autres patients atteints de POLG se sont depuis inscrits à l'essai clinique.
À propos de l’étude
L’étude Safety and efficacy of deoxycytidine/deoxythymidine combination therapy in POLG-related disorders: 6-month interim results of an open-label, single arm, phase 2 trial a été réalisée par Heather Pekeles, Saoussen Berrahmoune, Christelle Dassi, Anthony C.T. Cheung, Tommy Gagnon, Paula J. Waters, Ralf Eberhard, Daniela Buhas et Kenneth A. Myers.
L'étude a été principalement financée par la Fondation Liam, avec le soutien de la Fondation de l'Hôpital de Montréal pour enfants. Des fonds supplémentaires ont été reçus de la Fondation Savoy, de la Fondation du Grand Défi Pierre Lavoie et de donateurs privés.
DOI: https://doi.org/10.1016/j.eclinm.2024.102740
À propos de l’Institut de recherche du Centre universitaire de santé McGill
L’Institut de recherche du Centre universitaire de santé McGill (IR-CUSM) est un centre de recherche de réputation mondiale dans le domaine des sciences biomédicales et de la santé. Établi à Montréal, au Canada, l’Institut, qui est affilié à la faculté de médecine de l’Université McGill, est l’organe de recherche du Centre universitaire de santé McGill (CUSM) – dont le mandat consiste à se concentrer sur les soins complexes au sein de sa communauté. L’IR‑CUSM compte plus de 720 chercheurs et près de 1 400 étudiants et stagiaires qui se consacrent à divers secteurs de la recherche fondamentale, de la recherche clinique et de la recherche en santé évaluative au site Glen et à l’Hôpital général de Montréal du CUSM. Ses installations de recherche offrent un environnement multidisciplinaire dynamique qui favorise la collaboration entre chercheurs et tire profit des découvertes destinées à améliorer la santé des patients tout au long de leur vie. L’IR-CUSM est soutenu en partie par le Fonds de recherche du Québec – Santé (FRQS). www.ircusm.ca
À propos de l’Hôpital de Montréal pour enfants
Fondé en 1904, l’Hôpital de Montréal pour enfants (HME) est l’hôpital pédiatrique du Centre universitaire de santé McGill (CUSM). Premier hôpital du Québec à se consacrer entièrement aux soins des enfants, l’HME est un établissement d’enseignement et de recherche axé sur les soins de troisième et quatrième ligne aux nouveau-nés, aux enfants et aux adolescents de moins de 18 ans. L’HME dessert 63 % de la population géographique du Québec. Grâce à ses installations de soins et de recherche pédiatriques adjacentes à l’établissement pour adultes du site Glen, l’HME est dans une position unique pour offrir des services et réaliser des études aux différentes étapes de la vie de ses patients. Le Centre de médecine innovatrice — seul centre de recherche clinique en milieu hospitalier en Amérique du Nord — permet à ses chercheurs de mener des essais cliniques sur le site de l’hôpital. L’HME est un chef de file reconnu pour la prestation d’un vaste éventail de soins ultraspécialisés aux jeunes patients et à leurs familles de partout au Québec. L’hôpital est un centre provincial désigné de traumatologie reconnu pour la richesse de son expertise en cardiologie et en chirurgie cardiaque, en soins d’urgence, en neurologie et en neurochirurgie. https://hopitaldemontrealpourenfants.ca/
Personne-ressource pour les médias
Fabienne Landry
Coordonnatrice des communications, Recherche, CUSM
FabiennePraesent id dolor porta, faucibus eros vel.landry@muhc.mcgill.ca