
Breadcrumb
- News and Events
- News
- Content
- From silent infection to rapid death: Why are some people more vulnerable to COVID-19?
null From silent infection to rapid death: Why are some people more vulnerable to COVID-19?
Scientists discover genetic and immunological causes of 15 percent of life-threatening COVID-19 cases
September 25, 2020
Source: MUHC. Two studies published in Science by an international consortium of researchers provide a first answer to a crucial question: why does the individual vulnerability to COVID-19 vary so much in the population? The findings show that about 15 percent of patients who suffer from life-threatening COVID-19 have one thing in common: a defect in the activity of type I interferons (IFNs), molecules of the immune system that normally have a powerful antiviral activity. This defect is either caused by the presence of autoantibodies directed against those molecules or by genetic abnormalities that decrease their production. These findings could make it possible to detect people at risk of developing a severe form of the disease in all age groups and to better treat patients with these conditions.
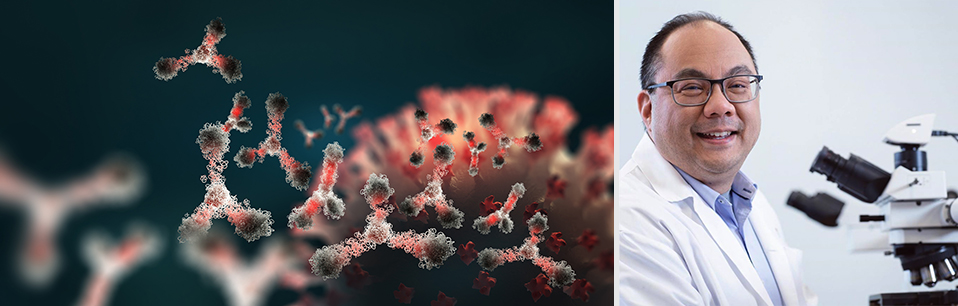
“Since the start of the pandemic, we saw that certain risk factors were associated with an increased risk for severe COVID-19: being male, elderly or having other medical conditions. However, the biological reason for why some of these groups were getting severe disease was not clear. Additionally, there were patients who did not have these risk factors – notably, young people – who were getting life-threatening COVID-19. Again, the reason why was far from understood,” explains Dr. Donald Vinh, clinician scientist in the Infectious Diseases and Immunity in Global Health Program at the Research Institute of the McGill University Health Centre (RI-MUHC), who participated in both studies. “Now, we understand that the disruption of a very important immune agent, type I interferon, is the cause of some of the worst cases of COVID-19.”
The findings are the first results being published out of the COVID Human Genetic Effort, an ongoing international project spanning over 50 sequencing hubs and hundreds of hospitals around the world, including the McGill University Health Centre. This initiative is co-led by Jean-Laurent Casanova, head of the St. Giles Laboratory of Human Genetics of Infectious Diseases at The Rockefeller University, and Helen Su, from the National Institute of Allergy and Infectious Diseases, in the United States.
Autoantibodies neutralizing type I interferons
Type I interferon is a set of 17 proteins crucial for protecting the body from viruses. Whether the proteins have been neutralized by autoantibodies or were not produced in sufficient amounts in the first place due to a faulty gene, the result is the same for a subgroup of COVID-19 patients: they struggle to fight the disease.
In the study Autoantibodies against type I IFNs in patients with life-threatening COVID-19, the scientists searched for autoantibodies against type I interferons in 987 patients hospitalized for life-threatening COVID- 19 pneumonia, 663 asymptomatic or mildly affected individuals infected with SARS-CoV-2, and 1,227 healthy controls from whom samples were collected before the COVID-19 pandemic.
They found that more than 10 percent of people who develop severe COVID-19 have misguided antibodies that attack not the virus, but the immune system itself, by blocking the action of type I interferon. These autoantibodies appear to be absent in people who developed a mild form of the disease, and they are rare in the general population.
“A striking element of this study is that these antibodies were much more present in men developing severe COVID-19, suggesting that their production could be linked to the X chromosome,” explains Dr. Vinh, who is also the director of the MUHC COVID-19 Biobank, an integral part of the Biobanque québécoise de la COVID-19, which collects biological materials and health information from COVID-19-positive people for research purposes.
The study suggests that patients with this profile may benefit from plasmapheresis (removal of the liquid portion of the blood containing white blood cells and antibodies) or other treatments that may reduce the production of these antibodies by B lymphocytes. Testing the general population for these antibodies could also help protect vulnerable individuals and may help predict, at the start of the infection, who may go on to develop severe COVID-19, allowing these people to get early antiviral treatment.
Inborn genetic errors decreasing the production of type I interferons
In the study Inborn errors of type I IFN immunity in patients with life-threatening COVID-19, the researchers genetically analyzed blood samples of 659 patients hospitalized for life-threatening COVID-19 pneumonia (14 percent of whom had died) and 534 subjects with asymptomatic or benign infection.
They discovered that at least 3.5 percent of patients with severe COVID-19 carry a specific kind of genetic mutation that diminishes their production of type I interferons. These mutations happen across 13 genes and are already known to be the cause of severe forms of influenza. Regardless of age, people with these genetic variations may be at greater risk of developing a potentially fatal form of influenza or COVID-19.
Early treatment with type 1 interferons could be a therapeutic option for these patients. These drugs have been available for more than 30 years and have no significant side effects if taken for a short period of time.