
Breadcrumb
- News and Events
- News
- Content
- Leading the way towards improved treatment for atrial fibrillation
null Leading the way towards improved treatment for atrial fibrillation
Always on the lookout for major developments in electrophysiology, MUHC clinical teams work closely with research teams at the RI-MUHC to offer the most innovative treatments to patients
SOURCE: MUHC
Atrial fibrillation is a condition that causes the upper chambers of the heart (called the atria) to beat irregularly and ineffectively. Affecting more than 60 million people worldwide, it is one of the most common cardiac disorders. A burden both for patients and the health system, it increases the risk of heart failure, stroke and death, and often worsens over time.
Antiarrhythmic drugs can often help control atrial fibrillation, but approximately half of the patients require minimally invasive surgical procedures to stop the electrical impulses that cause irregular heart rhythms. These procedures evolve as new technologies are developed, and the McGill University Health Centre (MUHC) has become a key player in Canada to test the latest approaches in atrial fibrillation management.
“At the MUHC, our teams in cardiology are committed to building clinical evidence for alternatives to drug therapy. Working with research teams at the RI-MUHC and with industry partners, our teams assess the latest and most promising minimally invasive ablation technologies to improve the health of our patients. What we do is unique in Canada,” says Dr. Atul Verma, director of the Division of Cardiology at the MUHC and a scientist in the Cardiovascular Health Across the Lifespan (CHAL) Program at the Research Institute of the McGill University Health Centre (RI-MUHC).
A rapidly advancing field
For the past twenty years, catheter ablation techniques have been used to improve treatment of atrial fibrillation. These techniques involve inserting tiny instruments into the heart through a vein or artery to apply heat or extreme cold where the arrhythmia is occurring, in order to create small scars in the heart tissue to stop the abnormal electrical signals that cause the arrhythmia. In recent years, however, new techniques have emerged.
“Though efficient, catheter ablation can sometimes lead to complications. Hence the development of new ablation technologies that we are currently evaluating in our translational lab and offering to our patients in clinical trials, such as pulsed field ablation, ultra-low temperature cryoablation and needle ablation,” explains Dr. Verma, who is a world-renowned cardiologist and cardiac electrophysiologist.
“Participating in such trials is crucial to the advancement of biomedical technologies and it also allows our patients to benefit from the latest advancements in the field,” adds Dr. Vidal Essebag, MUHC director of Cardiac Electrophysiology and a senior scientist in the CHAL program at the RI-MUHC.
Pulsed electric fields instead of heat
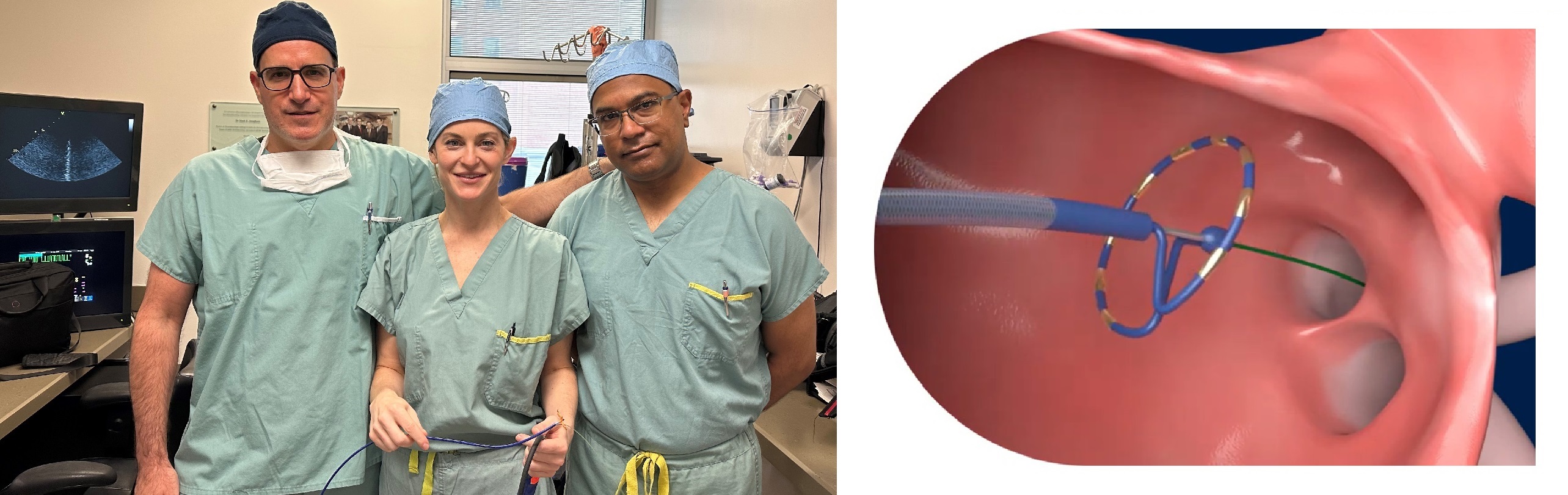
Recently, Dr. Verma was the leader of a global, multicentre clinical study that evaluated the safety and effectiveness of the Medtronic PulseSelectTM Pulsed Field Ablation (PFA) System – a technology that delivers pulsed electric fields instead of thermal energy to interrupt irregular electrical signals in the heart that trigger atrial fibrillation. It targets heart tissue with the goal of avoiding unwanted injury to surrounding tissues.
Conducted at 41 sites in nine countries (USA, Canada, Australia, Austria, Belgium, France, Japan, Netherlands and Spain), the study involved 300 patients who continued to suffer from atrial fibrillation despite taking medication to improve heart rhythm regulation and who were treated with this PFA system. More than half of them experienced no episode of atrial fibrillation in the year following the intervention. The results of the trial, published in March 2023 in the prestigious journal Circulation, demonstrated that the novel technology efficiency was comparable to the standard catheter ablation technologies, with a low rate of adverse events (0.7 per cent), one of the lowest ever achieved for any similar trial.
“We were able to show that this procedure is not only similarly efficient, but also faster and safer than thermal ablation,” says Dr. Verma, who is also an associate professor of Medicine at McGill University. “The findings from this trial could change how electrophysiology teams around the world treat atrial fibrillation.”
Furthermore, on May 15, MUHC teams successfully performed Canada's two first pulsed field ablation procedures using the new Farapulse technology from Boston Scientific, a technology that differs slightly from the one mentioned above, but that works on the same principle.
“It is too early to comment on long-term outcomes, but so far, these patients are doing very well,” says Dr. Verma.
Without the essential collaboration between clinical and research teams, MUHC patients would not have access to these novel technologies. They enjoy a better quality of life due to the exceptional competence and collaboration of the electrophysiology personnel at both the MUHC and the RI-MUHC.
“At the MUHC, we pride ourselves on providing the highest quality care and services possible to our patients. Providing access to novel technologies in our electrophysiology laboratory is an excellent example of how our interventional cardiology teams are leading the way in cardiac care services,” says Lucy Wardell, associate director of Nursing, Medical Mission, MUHC.
“I am very proud of our team and the work we are putting together for our patients,” adds Steeve Gaudreault, who was, until recently, the interim nurse manager in Interventional Cardiology at the MUHC, responsible for the Cath.Lab and the electrophysiology program. “The electrophysiology laboratory is a complex environment, where the team of nurses, medical radiation technologists, anesthesiologists and respiratory technicians must work together to deliver patient-centred care. The lab could never work successfully without each and every one of these individuals.”
"It is truly a pleasure to have our electrophysiology research team managed by Fiorella Rafti collaborate closely with our electrophysiology clinical team and our international fellows supervised by Dr. Martin Bernier. I also want to highlight the great contribution of Steeve Gaudreault and Stacey Mooney, the assistant nurse manager. Together, we provide world-leading excellence in patient care with the latest research and technologies," highlights Dr. Essebag.
About the publication
Verma A, Haines DE, Boersma LV, Sood N, Natale A, Marchlinski FE, Calkins H, Sanders P, Packer DL, Kuck KH, Hindricks G, Onal B, Cerkvenik J, Tada H, DeLurgio DB; PULSED AF Investigators. Pulsed Field Ablation for the Treatment of Atrial Fibrillation: PULSED AF Pivotal Trial. Circulation. 2023 May 9; 147(19):1422-1432. DOI: 10.1161/CIRCULATIONAHA.123.063988
July 5, 2023