
Breadcrumb
- News and Events
- News
- Content
- Multidisciplinary model improves hepatitis C care after release from prison
null Multidisciplinary model improves hepatitis C care after release from prison
New study from The Institute shows 70% increase in linkage to care through simple, team-based intervention
SOURCE: The Research Institute of the McGill University Health Centre
July 28, 2025
Amid global efforts to eliminate viral hepatitis, highlighted each year on World Hepatitis Day, new research from The Institute focuses on a population central to that goal: people transitioning out of prison without access to care. This population represents a critical gap in the global hepatitis response. Ensuring continuity of care after release from prison is an essential step toward achieving elimination targets set by the World Health Organization.
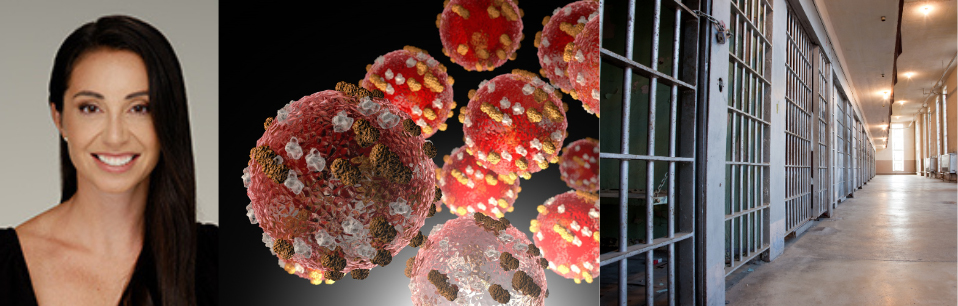
A new study led by Nadine Kronfli, MD, scientist at the Research Institute of the McGill University Health Centre (The Institute), demonstrates that a multidisciplinary team-based, person-centred model of care can dramatically improve access to hepatitis C (HCV) treatment for individuals transitioning out of the prison system untreated.
The Beyond Prison Walls study, published in the International Journal of Drug Policy, was conducted at Quebec's largest provincial prison and followed people with untreated HCV after their release. The research team compared two approaches: one group received standard care, consisting of a single pre-release discharge appointment; the other was enrolled in a new multidisciplinary program that involved a nurse, social worker, and patient navigator, with structured follow-up and appointment accompaniment in the community.
"Many people leaving prison have multimorbid health care needs but face overwhelming barriers to care," said Dr. Kronfli. "This study shows that with the right support — including care coordination and follow-up — we can dramatically increase access to treatment following release from prison. It's a scalable model with real potential to close one of the biggest gaps in hepatitis C care."
The findings were striking: 80 percent of participants in the intervention group were linked to HCV care within 90 days of release, compared to just 11 percent in the control group — a 70 percent increase. This proportion linked to HCV care is higher than those observed in similar studies from the United States and Australia, marking a significant advancement in the field of carceral and transitional health care.
The success of the model hinged on proactive outreach and consistent contact after release. Participants who were successfully reached by the care team — whether directly or through their emergency contact network — were 64 percent more likely to be linked to HCV care. The inclusion of a patient navigator - who accompanied participants to appointments and coordinated follow-up - also proved vital. All transportation costs were offset, removing an important barrier to post-release care.
The Beyond Prison Walls model of care, staffed by trained health professionals, was integrated into the existing correctional health infrastructure at the largest provincial prison in Quebec. It was designed to be scalable across provinces and countries, and sets a new standard for transitional care for hepatitis C after community re-integration.
What's next
A cost-effectiveness study of the Beyond Prisons Walls model of care is currently under review. Results suggest that the model is financially sustainable, further supporting global scale up. As jurisdictions move toward hepatitis elimination, this study shows that providing transitional care from prison-to-community is not only possible—it is essential.
About the study
"A pre-post study of the impact of a multidisciplinary model of care on linkage to hepatitis C care following release from prison: The Beyond Prison Walls study" by Nadine Kronfli, Andrea Mambro, Allen O'Brien, Camille Dussault, Sylvie Chalifoux, Lina Del Balso, Apostolia Petropoulos, Mona Lim, Alexandros Halavrezos, Bertrand Lebouche, Giada Sebastiani, Marina Klein and Joseph Cox was published in the International Journal of Drug Policy.
doi: 10.1016/j.drugpo.2025.104873
The study was funded by the Canadian Institutes of Health Research (CIHR), Gilead Sciences, and the MUHC Foundation.
Related News
RI-MUHC researcher receives federal funding to improve health outcomes in Quebec prisons