- Home /
- About Us /
- Annual Reports /
- Annual Report 2023 /
- Connected for discovery
RI-MUHC ANNUAL REPORT 2023
CONNECTED FOR DISCOVERY: HOW TEAM SCIENCE RAISES THE BAR
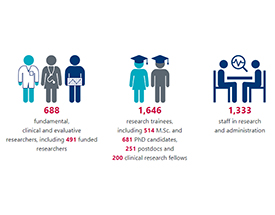
Building connections for team science creates a powerhouse for discovery. At the Research Institute of the McGill University Health Centre (RI-MUHC), we recognize that the most impactful research is grounded in our networks of expertise: the vital connections our researchers forge with other scientists and healthcare practitioners of diverse perspectives, whether from across the hallway, across Canada, or from one of the 70 countries in our worldwide network of collaborations. We nurture these connections to accelerate discovery and knowledge translation so that we may fast-forward to a world in which more diseases can be cured, personalized medicine is within reach for all, and, with more equitable access to treatments, more people can live healthier lives.
In this feature, eight of our researchers explain how team science helps them to aim high and advance toward the most ambitious goals in health care research.

- In research and in patient care, the only way to go far is to go together (Sherif Emil)
- Improving health outcomes for mother and child, on a broader scale (Sushmita Pamidi)
- Expediting innovation in anesthesia and surgery (Thomas Hemmerling)
MEETING INDIVIDUAL AND GLOBAL NEEDS
- Valuing diversity is the mainstay in personalized medicine (Louise Pilote)
- Meeting the mental health needs of Canadians across the lifespan (Deborah Da Costa)
PUSHING THE FRONTIERS OF FUNDAMENTAL RESEARCH
- Cracking the nanoscopic structural code of the healthy and diseased brain (Keith Murai)
- Deciphering the complex biology of pediatric cancers (Livia Garzia)
- Admitting one’s limitations may be the precursor to discovery (Janusz Rak)
DRIVERS OF CLINICAL RESEARCH
In research and in patient care, the only way to go far is to go together

A significant culture change in medicine during the last few decades has been the adoption of multidisciplinary care. Given the increasing complexity of medical and surgical care, the age of a single physician or medical specialist attending to a patient's medical care is well behind us. It has become clear that we must collaborate, create teams, and coordinate care if we are to administer the best in medical and surgical care in the twenty-first century.
The same applies to medical research. Perhaps no specialty demonstrates that better than mine: pediatric surgery. This niche specialty, characterized by rare diseases, has seen a major shift in research output over the last decade, moving from single-centre retrospective studies to higher quality studies performed through collaborations with other disciplines, and conducted through research consortia.
In Canada, we have created the Canadian Consortium for Research in Pediatric Surgery (CanCORPS), anchored at the RI-MUHC. This consortium has already set an international example for how to bring teams together and has produced team-science based work that will change practice, improving patient care and optimizing resource utilization.
CanCORPS recently assembled a team to perform a prospective study to improve the care of children who suffer the most common acute surgical illness, appendicitis. The team members are from 10 medical and surgical disciplines, in addition to epidemiologists, health services researchers, and statisticians from 11 centres across Canada, as well as international centres in the United States, the United Kingdom, the Netherlands and Brazil. This is the power of team science, and it can only be realized through the resources of an organization such as the RI-MUHC. I spend quite a bit of time each year in global surgical work, where we often repeat an African proverb: “If you want to go fast, go alone. If you want to go far, go together.” I believe this also applies to our efforts as investigators. The only way to go far is to go together.
Sherif Emil, MDCM, FRCSC, FACS, FAAP
Investigator, Child Health and Human Development Program, RI-MUHC

Related news
The Canadian Consortium for Research in Pediatric Surgery: Roadmap for Creation and Implementation of a National Subspecialty Research Consortium
A new research study may reduce surgical interventions for baby girls
CanCORPS website
Improving health outcomes for mother and child, on a broader scale
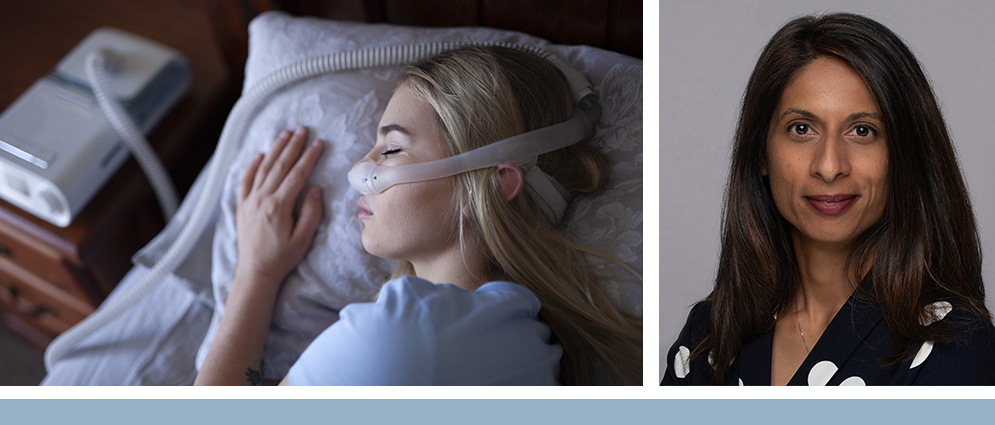
The overall aim of my research program has been to determine whether maternal sleep-disordered breathing (SDB) during pregnancy is associated with adverse health consequences for the mother and child. Team science plays a crucial role in advancing our research in various areas, including SDB and its association with cardiometabolic disorders, as well as innovative treatment approaches for pregnancy and sleep-disordered breathing.
Building upon our collaboration with investigators in the 3D Cohort, a Quebec pregnancy and birth cohort led by Dr. William Fraser (Université de Sherbrooke), my team contributes to a unique cross-disciplinary research collaboration across Quebec, encompassing adult and pediatric sleep medicine and cardiometabolic disorders. Pooling resources, knowledge and methodologies, we are able to conduct a follow-up study of mothers and children approximately 10 years after delivery and examine the long-term effects of sleep-disordered breathing (SDB) on cardiometabolic health.
Building upon our recent work that highlighted the negative effects of untreated severe SDB on glucose control in individuals with gestational diabetes, we have been pursuing a patient-preference approach to treatment of SDB. Recently, we obtained a CIHR Project Grant with patient partners as collaborators and co-investigators at London Health Sciences Centre to better understand the barriers and facilitators to treating SDB in pregnancy. With patient partners and sleep-dental colleagues, we have also designed a novel clinical trial to address the importance of tailoring treatment options to individual preferences and choices. Moreover, as co-principal investigator for the multisite Accelerating Clinical Trials (ACT) Canada Consortium CIHR clinical trials grant led by P.J. Devereaux (McMaster University), and as co-chair for the ACT RI-MUHC clinical trial unit, I work with a diverse group of scientists from various backgrounds across the country to improve how we conduct clinical trials at the RI-MUHC and in Canada.
Through such collaborations with diverse scientists, we expand our knowledge base, increase the generalizability of our findings, and contribute to improving health outcomes on a broader scale. In this way, we may provide the best possible returns to our funding partners at the CIHR, FRQS and other agencies, and to our own dedicated McGill University Health Centre foundations.
Sushmita Pamidi, MD, M.Sc.
Scientist, Centre for Outcomes Research and Evaluation, and co-leader, Translational Research in Respiratory Diseases Program, RI-MUHC
Related news
Significant funding to maximize access and drive excellence in clinical trials in Quebec and Canada
Expediting innovation in anesthesia and surgery

As the director of the Intelligent Technologies in Anesthesia Group (ITAG) at the RI-MUHC, I can confidently affirm the profound impact that team science brings to our research. The fusion of distinct perspectives and broad expertise within our team fast-tracks scientific innovation and facilitates the translation of our findings into actionable solutions.
Our team, composed of anesthesiologists, engineers and artificial intelligence (AI) specialists, represents a diverse array of knowledge. This synergy has been instrumental in propelling us into multiple pioneering fields. We have been able to delve into the realms of automated drug delivery, surgical simulators, and other significant areas of technological innovation in anesthesia and surgery. These explorations would not have been possible without the power of our multidisciplinary collaboration.
Team science enables us to tackle complex issues from multiple angles and cultivates a culture of lifelong learning among our team members. As we share our unique experiences and insights, we collectively expand our understanding of the challenges and opportunities within multiple fields. This dynamic interplay of ideas encourages an intellectually stimulating environment that continually propels our research forward.
In essence, team science acts as the lifeblood of our research endeavours. The collaboration and connectivity fostered through this approach is what propels us towards innovative discoveries and their effective translation into practice. Through this collective effort, we aim to continue making significant strides in anesthesia, surgery and perioperative medicine.
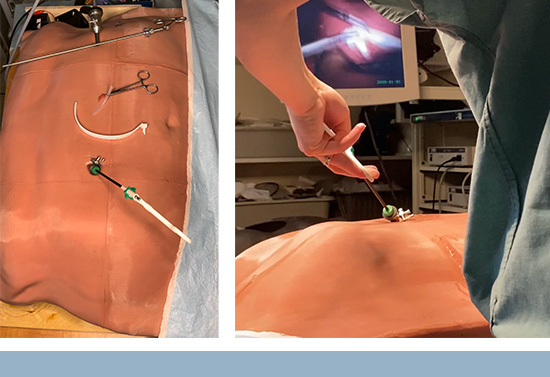
Thomas Hemmerling, MD
Senior scientist, Injury Repair Recovery Program, RI-MUHC
Related news
CQDM funds a collaborative research project between the RI-MUHC and Divocco AI
MEETING INDIVIDUAL AND GLOBAL NEEDS
Valuing diversity is the mainstay in personalized medicine

I can attest to the transformative power of team science in our research. My work, at the intersection of sex, gender, and cardiovascular health, demands a rich interplay of perspectives and skillsets that can only be facilitated by collaborative research.
Our flagship initiative, the Gender Outcomes International Group to Further Well-being Development (GOING-FWD), is a testament to the strength of team science. This consortium has assembled thirty investigators from five countries, each contributing unique insights and methodologies to understand the intricate relationship between sex, gender and health outcomes in 30 million patients with chronic diseases.
The perspectives that each member brings to this work broadens our collective understanding and leads us towards innovative solutions. Cross-cultural comparisons help us grasp how social determinants of health that are gendered and biological factors vary across different populations. We leverage big data and utilize the power of artificial intelligence (AI) and machine learning in collaborations that would be impossible without the convergence of minds from different disciplines.
Our collaboration does not stop within the confines of our team. We also engage with stakeholders, including policymakers and patients. This is an essential aspect of team science – integrating diverse insights, not only from scientists but also from those directly affected by research outcomes.
A recent publication by our GOING-FWD consortium showcases the benefits of this team science approach. Published in BMJ Global Health in April 2021, the paper describes how the diverse expertise and perspectives of our researchers, along with input from patients, can address the significant gap in assessing gender-related factors as health determinants.
Collaborative, interdisciplinary research not only accelerates scientific discovery but also broadens its impact, fostering a holistic understanding of health and disease. This approach is fundamental in creating personalized interventions that reflect patients' unique experiences, realities and needs.
Louise Pilote, MD, MPH, PhD
Senior scientist, Cardiovascular Health Across the L ifespan Program and Centre for Outcomes Research and Evaluation; interim director, Centre for Innovative Medicine; and co-deputy executive director/chief scientific officer, RI-MUHC

Related news
Identification and inclusion of gender factors in retrospective cohort studies: the GOING-FWD framework (BMJ Global Health)
Significant funding to maximize access and drive excellence in clinical trials in Quebec and Canada
Big start for the Canadian Mother-Child Collaborative Training Platform – CAMCCO-L
Meeting the mental health needs of Canadians across the lifespan

The research projects underway in my lab seek to better understand the mental health challenges faced by individuals across their lifespan and to identify modifiable factors that help preserve and promote mental well-being. We use this knowledge to develop scalable digital health interventions that promote mental health, using a gender lens.
My research program benefits from collaborations with experts across multiple disciplines to successfully answer and address these important research questions. My recently funded study brings together a multidisciplinary Canadian team of perinatal health experts to evaluate an engagement-enhanced digital intervention targetting the mental health of at-risk new fathers.
Comprised of clinicians, researchers, community providers and knowledge users, this team promotes collaborations across six disciplines: psychology, psychiatry, dietetics, nursing, kinesiology, and digital health technology.
Seeking out and establishing connections with experts across fields is essential to advance knowledge and make an impact in research areas where gaps in our understanding continue to exist. With my interdisciplinary team, knowledge can be applied to make evidence-based changes to practice and policies in an equitable and inclusive manner, better meeting the mental health needs of Canadians across the lifespan.
Deborah Da Costa, PhD
Scientist, Child Health and Human Development Program and Centre for Outcomes Research and Evaluation, RI-MUHC
Related news
New funding to support Canadian veterans and their families
PUSHING THE FRONTIERS OF FUNDAMENTAL RESEARCH
Cracking the nanoscopic structural code of the healthy and diseased brain
The human brain is among the most fascinating, yet enigmatic, biological structures known to humankind. The brain enables us to learn, communicate, and experience the world around us. Decreases in brain function – for example, following stroke or associated with a neurodegenerative disease such as Alzheimer’s disease – can significantly impact our mental and physical well-being, as well as the ability to function independently and contribute to society. However, understanding how the brain works in healthy and disease states has been extremely challenging due to the complex nature of brain cells and their connections. This is where a team science approach is necessary to decode the brain’s intricate structural properties.
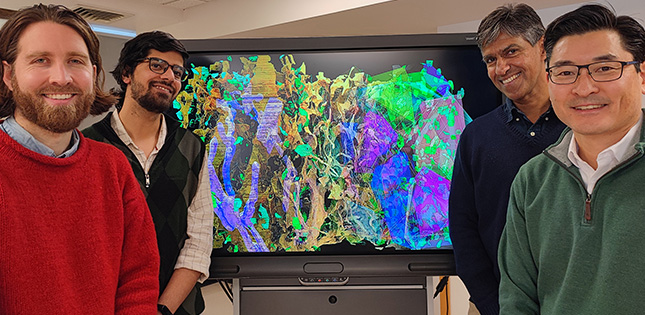
Over the last five years, our lab has drawn upon the expertise and perspectives of neuroscientists, anatomists, imaging specialists, computer scientists and mathematicians to develop new, powerful computer vision and machine learning approaches to decode the complex nanoscopic structural framework of brain cells in their native three-dimensional environment. By deploying new imaging technologies, three-dimensional modeling and computational approaches to resolve brain structure, we were able to discover an unexpected level of complexity in how brain cells are constructed, organized, and interact with one another. These findings have permitted exciting new ways to examine and quantify the cellular fabric of the brain and how it changes following injury or disease.

A key aspect of our research is the creation of a new generation of “multilingual” trainees who have crossed the pedagogical and experimental boundaries of multiple scientific disciplines and are able to develop and harness new technologies and approaches such as computer vision, a branch of artificial intelligence, to decipher the structural code of the healthy and diseased brain.
Keith Murai, PhD
Senior scientist and leader of the Brain Repair and Integrative Neuroscience Program, RI-MUHC
Related news
RI-MUHC and McGill researchers make a breakthrough in understanding brain nanoarchitecture, using computer vision
Un financement novateur de trois chaires doubles en Intelligence artificielle en santé / Projets chaires doubles (French only)
Deciphering the complex biology of pediatric cancers
Sarcomas and brain tumours are among the most common malignant solid cancers in children, adolescents and young adults. These cancers can be deadly in young people, but they are diagnosed less frequently than cancers in adults. Overall, outcomes are more successful than was the case a few decades ago, but methods of diagnosing and treating these cancers have not progressed quickly enough. Too many patients still die or are over-treated. These failures are caused by the complex biology of these cancers, in which specific processes that are typical of young cells are hijacked and twisted to fuel the growth of tumours.

Multidisciplinary research teams offer the best hope for health research at this level of complexity. Such teams, often composed of twenty to thirty scientists, result in faster and more efficient dissemination of new discoveries and treatment possibilities to researchers, clinicians and the public. These important benefits may be expanded further, as we find that new developments in one area can be relevant, unexpectedly, t o other medical fields. In a study that our group published this year, for instance, with a team composed of clinician scientists in the field of pediatric oncology, neuroscientists, and computational and big data scientists, we discovered that a mutation commonly found in brain tumours can also have a causal role in rare, genetically driven neurodegeneration.
Through multidisciplinary research teams, novel ideas can be developed from scratch and tested quickly. With this approach, new technologies can be refined in real time to achieve maximum effect. This is the aim of our recent project on liquid biopsies in pediatric cancers, which brings together computational scientists, bioengineers, pediatric oncologists and molecular biologists to devise new ways to monitor cancer progression or regression in young patients, by using blood tests.
Livia Garzia, PhD
Scientist, Cancer Research Program, RI-MUHC
Related news
Too much pruning: A new study sheds light on how neurodegeneration occurs in the brain
Liquid biopsy research: a generous boost to help children with cancer
Admitting one’s limitations may be the precursor to discovery

A lone scientist working in an ivory tower has never been the reality of health research, and this imagined stereotype is particularly untrue now. Science, discovery and innovation have always been based on connections, a dialogue of minds – those of the past, present and future – all reference points that define progress. In the highly complex world of today’s health research, in my case cancer research, the increasing drive for deeper knowledge and rapidly applicable solutions challenges the limits of an individual’s expertise and stimulates interactions, interdependencies and synergies.
Despite some barriers to integration, such as the academic culture rewarding individual successes, there are many rewards, both personal and professional. Team science sparks mutual learning, the satisfaction of getting things done together, and often, lasting professional friendships. My long-standing interest in the role of cell-cell communication in the pathogenesis of cancer and the related therapeutic and diagnostic opportunities, such as extracellular vesicle-based liquid biopsy, has made me acutely aware of my own limitations. I have had the good fortune of meeting expert colleagues with different perspectives, which has opened my eyes to the wonders and power of biobanking, translational oncology, genomics, computation biology and nanotechnology. All of these have gradually become absorbed into my own team’s research program, coalescing with the work of colleagues.
The Centre for Applied Nanomedicine and pediatric Liquid Biopsy Research Project are two examples of independently funded, highly gratifying and productive synergies among multiple researchers catalyzed by our group. The RI-MUHC is the home for these and other thriving initiatives whose reach extends through international collaboration, gaining ground in our search for a better, healthier life.
Janusz Rak, MD, PhD
Senior scientist, Child Health and Human Development Program, RI-MUHC
Related news
Liquid biopsy research: a generous boost to help children with cancer
Exosomes, vesicles and particles are no longer obscure