
Breadcrumb
- News and Events
- News
- Content
- All airway trees are not created equal
null All airway trees are not created equal
An RI-MUHC study suggests that lung development in early life has an impact on the risk of premature death
Montreal, July 20, 2023 – People with smaller airways relative to the size of their lungs - a condition called dysanapsis - could die sooner than others. In particular, they could be more at risk of dying from chronic obstructive pulmonary disease (COPD), lung cancer and atherosclerotic cardiovascular disease (ASCVD) – the three leading causes of death that are linked to smoking and air pollution.
These are the main findings of a prospective study conducted at the Research Institute of the McGill University Health Centre (RI-MUHC) among a multi-ethnic cohort of over 6,500 adults. The study, which has important implications for lung health in the 21st century, was recently published in the European Respiratory Journal.
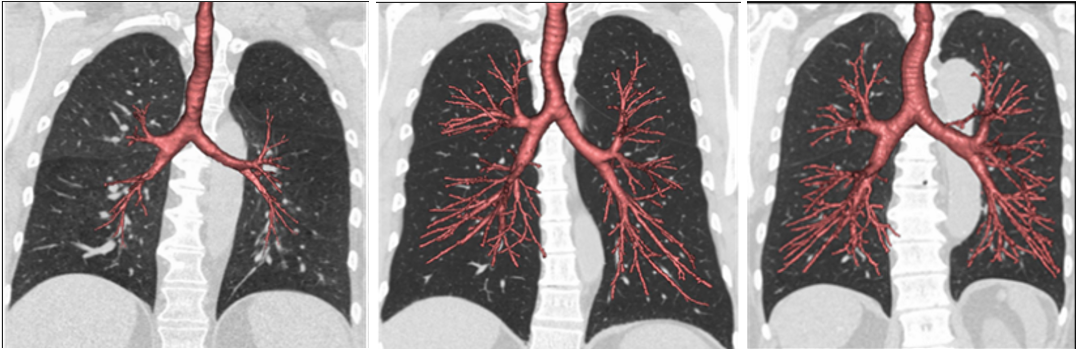
Dysanapsis corresponds to a developmental mismatch between the airway tree and lung size that can be assessed by CT scan and observed in early adulthood. As people grow, their airways normally develop in proportion to their lungs, but in some people, the airways do not get as large as expected.
"Previous studies have demonstrated associations between lung structure and mortality among heavy smokers, where lung structure may reflect the cumulative effects of smoking. Our study now demonstrates associations between native lung structure and mortality in a general population sample, including among never-smokers," explains Dr. Benjamin Smith, senior author of the study and a scientist in the Translational Research Program in Respiratory Diseases at the RI-MUHC.
Smaller airways, higher risk of death
This study included over 6,500 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), a cohort that includes men and women from six different regions of the USA, who had a mean age of 62 years when they enrolled in the study, in the year 2000.
Study participants were followed from 2000 to 2018 and were classified into four quartiles according to their airway-to-lung ratio, from small to large. On the dysanapsis spectrum, a small airway-to-lung ratio refers to an individual with smaller airways than normal, and a high ratio refers to an individual with larger airways than normal.
Overall, there were 1,635 deaths, including 232 from ASCVD, 128 from lung cancer and 59 from COPD.
The researchers found that the lower the airway-to-lung ratio, the higher the number of deaths (515 deaths in the lowest quartile, versus 323 in the highest). There were 60.1 excess deaths per 10,000 person-years (equivalent to 1,000 people followed for 10 years) in the smallest quartile compared to the largest – indicating a significantly higher all-cause mortality.
An association that remains true among non-smokers
Strikingly, the association between a small airway-to-lung ratio and higher mortality was evident in both never-smokers (35.8 excess deaths per 10,000 person-years) and ever-smokers (94.3 excess deaths per 10,000 person-years).
"The associations we observed between smaller airway-to-lung ratio and higher mortality were independent of demographics, body size and potential confounding factors, such as racial or ethnic ancestry, and exposure to air pollution and tobacco,” notes Dr. Motahareh Vameghestahbanati, first author of the study, internal medicine resident and recipient of the prestigious Vanier Canada Graduate Scholarship and McGill MedStar Award for Trainees.
“These new findings suggest that excess mortality associated with airway structure is not due exclusively to smoking-induced structural changes, and may instead result from a developmental trait that increases susceptibility to death from pulmonary and non-pulmonary conditions," adds Dr. Vameghestahbanati, who recently completed her PhD at the RI-MUHC.
“This is the first study to examine the relationship between measures of airway lumen calibre and mortality in the general population and, notably, among non-smoking individuals," emphasizes Dr. Smith, who is also a respirologist at the Montreal Chest Institute of the MUHC and an associate professor in the Department of Medicine at McGill University.
“A provocative implication of this work is that it provides evidence that “all airway trees are not created equal” vis-à-vis susceptibility to inhaled noxious aerosols (e.g. tobacco smoke, air pollutants), opening research avenues to understand and promote resilient lung development and maintenance across the lifespan,” he adds.
These results build on other important discoveries in respiratory medicine emanating from the RI-MUHC in recent years. A study led by Dr. Smith and published in JAMA in 2020 showed that dysanapsis was an important risk factor for COPD and that people with larger airways seemed more resistant to respiratory disease. Another study, published in 2022 in the American Journal of Respiratory and Critical Care Medicine, showed that dysanapsis increased vulnerability to the long-term effects of air pollution on respiratory function.
About the study
The study Association of dysanapsis with mortality among older adults was conducted by Motahareh Vameghestahbanati, Coralynn Sack, Artur Wysoczanski, Eric A. Hoffman, Elsa Angelini, Norrina B. Allen, Alain G. Bertoni, Junfeng Guo, David R. Jacobs, Joel D. Kaufman, Andrew Laine, Ching-Long Lin, Daniel Malinsky, Erin D. Michos, Elizabeth C. Oelsner, Steven J. Shea, Karol E. Watson, Andrea Benedetti, R. Graham Barr and Benjamin M. Smith
DOI: 10.1183/13993003.00551-2023
About the Research Institute of the McGill University Health Centre
The Research Institute of the McGill University Health Centre (RI-MUHC) is a world-renowned biomedical and healthcare research centre. The institute, which is affiliated with the Faculty of Medicine of McGill University, is the research arm of the McGill University Health Centre (MUHC)—an academic health centre located in Montreal, Canada, that has a mandate to focus on complex care within its community. The RI-MUHC supports over 450 researchers and around 1,200 research trainees devoted to a broad spectrum of fundamental, clinical and health outcomes research at the Glen and the Montreal General Hospital sites of the MUHC. Its research facilities offer a dynamic multidisciplinary environment that fosters collaboration and leverages discovery aimed at improving the health of individual patients across their lifespan. The RI-MUHC is supported in part by the Fonds de recherche du Québec — Santé (FRQS). rimuhc.ca
Media contact
Fabienne Landry
Communications coordinator, Research, MUHC
FabiennePraesent id dolor porta, faucibus eros vel.landry@muhc.mcgill.ca
514 812-7722