
Fil d'Ariane
- Nouvelles et événements
- Nouvelles
- Content
- Contrer la réticence face à la vaccination
null Contrer la réticence face à la vaccination
Notre meilleur espoir de tracer la voie à un monde post-pandémique
Par Ian Popple
Source : Le Bulletel. Après avoir réalisé l’exploit monumental de développer et d’approuver, non pas un, mais deux vaccins contre la COVID-19 en moins d’un an, l’heure est maintenant à la vaccination – sans doute la phase la plus cruciale de la pandémie jusqu’à présent. « Garantir une distribution efficace et équitable de ces vaccins est notre meilleur espoir de tracer la voie à un monde post-pandémique », affirme le Dr Don Sheppard, directeur du Département de microbiologie et d’immunologie de la Faculté de médecine et des sciences de la santé de l’Université McGill, et directeur de l’Initiative interdisciplinaire en infection et immunité de McGill (MI4).
Ne pas réussir à administrer le vaccin à assez de personnes pour obtenir une immunité collective – ce moment où le virus ne trouve plus assez d’hôtes pour se propager – serait comme chuter à la ligne d’arrivée d’un marathon. Il existe pourtant des obstacles importants à la vaccination, allant des défis logistiques de la distribution à la résistance du public enracinée dans les mentalités culturelles.
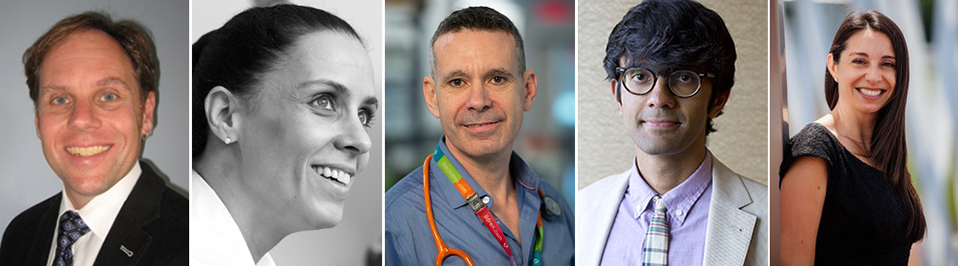
Surmonter ces obstacles dans un contexte réel
« MI4 a lancé un appel à propositions à l’automne dans le but de développer des stratégies pour surmonter ces obstacles dans un contexte réel », explique le Dr Sheppard, qui est également scientifique senior dans le Programme en maladies infectieuses et immunité en santé mondiale à l’Institut de recherche du Centre universitaire de santé McGill (IR-CUSM). Six études ont été sélectionnées et ont reçu des subventions de MI4 allant jusqu’à 100 000 $ chacune, grâce aux efforts de financement de la Fondation du Centre universitaire de santé McGill (CUSM), de l’unité Avancement universitaire McGill et de la Fondation de l’Hôpital général juif, qui sont fières de voir leurs chercheurs dynamiques et les communautés apparentées collaborer sous l’égide de MI4.
Quand on pense à ce que le monde a vécu au cours de la dernière année, il semble inconcevable que quiconque soit réticent à adopter une solution potentielle. Pourtant, des études suggèrent que plusieurs restent sceptiques face à la vaccination. Des recherches publiées l’automne dernier ont montré que seuls 39 % des Canadiens se feraient vacciner dès qu’un vaccin serait disponible, contre 46 % en juillet.
« Voie rapide » ne veut pas dire « raccourci »
L’une des raisons qui expliquent cette réticence est l’insécurité liée à la vitesse à laquelle ces vaccins ont été mis au point. Les vaccins mettent généralement entre 10 et 15 ans à arriver sur le marché. Dans les années 1960, le compteur a été réinitialisé avec le vaccin contre les oreillons, qui a été créé en à peine quatre ans. Mais la propagation rapide de la COVID-19, et le nombre vertigineux de décès, ont permis d’accélérer le développement de plusieurs vaccins en un temps record. « Plusieurs aspects du processus d’approbation, comme les examens administratifs, ont été lancés tôt pour ne pas retarder le processus, et des usines ont été construites pour produire le vaccin en grande quantité alors qu’il était toujours en développement, explique le Dr Sheppard. Il est important que les gens comprennent que “voie rapide” ne veut pas dire “raccourci”. »
Malheureusement, comme le veut le dicton, un mensonge peut faire le tour de la terre le temps que la vérité mette ses chaussures. C’est encore plus vrai aujourd’hui avec la fausse information qui peut être partagée à travers les réseaux sociaux d’un seul clic. « La réticence face aux vaccins est, dans une large mesure, enracinée dans le manque de confiance envers les institutions sociales, dont la science elle-même », rapporte le Pr Ian Gold, des départements de philosophie et de psychiatrie de l’Université McGill, qui dirige l’un des nouveaux projets de MI4. L’étude du Pr Gold vise à surmonter ce problème en développant une stratégie basée sur la confiance pour augmenter l’adhésion aux vaccins. La Dre Inés Colmegna, professeure agrégée à l’Université McGill rattachée à la Division de rhumatologie du CUSM, cherche pour sa part à répondre aux craintes et aux idées fausses similaires en adaptant les stratégies tirées des campagnes de vaccination contre la grippe.
Les autres études de MI4, financées par la nouvelle initiative, visent des groupes démographiques précis. Une étude menée par le Dr Zeev Rosberger, professeur agrégé aux départements d’oncologie, de psychiatrie et de psychologie de l’Université McGill et chercheur sénior à l’Institut Lady Davis de l’Hôpital général juif, a pour ambition d’encourager les comportements altruistes chez les 20 à 40 ans, relativement peu exposés. Le Dr Moshe Ben-Shoshan, professeur adjoint en pédiatrie à l’Hôpital de Montréal pour enfants, dirige une étude centrée sur les enfants, et le Dr Abhinav Sharma, professeur adjoint à l’Université McGill rattaché à la Division de cardiologie du CUSM, vise à encourager la vaccination des patients atteints de maladies cardiovasculaires et d’autres personnes à haut risque.
Des interventions qui pourraient augmenter le taux d’adhésion
Le dernier des six projets nouvellement financés vise à faire la lumière sur la propagation du coronavirus dans les établissements correctionnels du Canada – un secteur auquel on a accordé trop peu d’attention. « Les prisons sont des milieux collectifs très semblables aux établissements de soins de longue durée, où le virus peut se propager facilement entre les détenus, les gardiens, le personnel de soutien et les communautés environnantes », explique la chercheuse principale, Dre Nadine Kronfli, professeure adjointe à l’Université McGill, rattachée à la Division des maladies infectieuses du CUSM. « Bien que les taux de vaccination aient été historiquement bas dans les prisons canadiennes, des études ont montré que les programmes de vaccination peuvent augmenter le taux d’adhésion s’ils sont associés à une intervention éducative ». La Dre Kronfli va déterminer la forme que devrait prendre cette intervention éducative pour être efficace, et notamment le messager idéal pour transmettre l’information. Des éléments donnent à penser que ce sont les infirmières ou les pairs des détenus qui sont peut-être les mieux placés pour jouer ce rôle dans les établissements pénitentiaires.
Chacune de ces études a une durée de six mois seulement, ce qui devrait permettre de tirer des informations concrètes et exploitables des résultats afin d’améliorer le programme de vaccination du Canada cette année même, et ainsi aider à mettre fin à la pandémie. Comme l’explique le Pr Gold : « Ces vaccins contre la COVID-19 ont fait beaucoup de chemin depuis les laboratoires où ils ont vu le jour, mais cet effort sera impuissant à contrer la pandémie s’ils ne se rendent pas dans le bras des receveurs. »
26 janvier 2021