- Home /
- Research /
- Programs /
- Metabolic Disorders and Complications /
- Themes

MeDiC | Metabolic Disorders and Complications Program
MeDiC
RESEARCH PROGRAMS
Themes
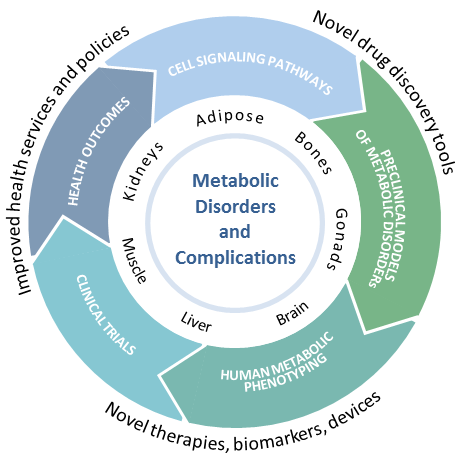
The Metabolic Disorders and Complications (MeDiC) Program integrates outstanding basic science with leading-edge clinical and evaluative research. With expertise in all facets of clinical investigation and knowledge translation, our program addresses highly prevalent diseases exerting enormous morbidity and economic burden on society: obesity and overweight (39% of population); diabetes (8.5% of population); osteoporosis (1 in 3 women and 1 in 5 men will sustain fractures ); and chronic kidney disease (10% of population). This work is organized within five major research themes. Each theme incorporates research from multiple disciplines and stimulates frequent interaction with other RI-MUHC research programs.
Energy metabolism


Obesity is the main driver of the global epidemic of diabetes. The MeDiC Program is exploring novel concepts with concern for causes as well as cures. In vivo hyperinsulinemic clamp methods, previously used for research phenotyping, are being translated into novel therapy in the perioperative management of cardiac surgery patients, yielding improved postoperative outcomes. Applying a systems biology approach to human liver samples, we are exploring the molecular pathogenesis of non-alcoholic fatty liver disease to identify novel drug targets for this nonclassical complication of diabetes and obesity. We are identifying new targets (e.g., proteins and signalling pathways) that will help lead to new treatments to prevent high glucose-induced kidney injury, leading to better health and longer life for people with diabetes. We are a major site of clinical trials in diabetes, the only islet cell transplantation program in Eastern Canada, and developing a world-leading closed loop bihormonal insulin/glucagon pump.


Since a change in health behaviour is the most effective method of preventing the onset of diabetes in obesity, we are developing and testing strategies that integrate new technology (apps, wearable devices) that can be used to overcome the barriers to increasing physical activity in type 2 diabetes, gestational diabetes, obesity, and pregnancy. We are developing online resources and intervention platforms to improve eating behaviours and deliver cognitive behavioural therapy.
Metabolic disorders and the brain

Disordered metabolism (e.g., obesity, diabetes, uremia, musculoskeletal fragility) adversely affects the brain, particularly by increasing the risk of cognitive dysfunction. We are building on a number of projects in the area of the interaction of metabolic disorders and the brain. We are using novel in vivo imaging methods to define new paradigms in the fundamental mechanisms by which the hypothalamus regulates both appetite and energy expenditure to defend the set point for body weight, and how these mechanisms can be altered by overfeeding, physical activity, drugs and irradiation. Our work on hypothalamic plasticity in regulating metabolism has led to the development of novel imaging methods of specific neurons repeatable over time in live mice. Such tools are useful not only for elucidating physiology and pathophysiology, but also for evaluation of drug efficacy/toxicity in the central nervous system. We are applying Functional magnetic resonance imaging (fMRI) for imaging of the brain and metabolomic profiling to further develop our observations of efficacy of high-dose intravenous insulin during cardiac surgery to prevent postoperative decline in cognitive function.
We are studying the biology of aging and the mechanisms underlying Parkinson’s (PD) and Huntington’s (HD) disease to develop novel treatments for age-onset neurodegenerative disease. By translating benchside knowledge, we aim to propose novel therapeutic strategies to target progressive spreading of pathogenic protein aggregates and treat PD. Our additional work on effects of metabolism on cognitive dysfunction, progranulin and dementia, sarcopenia and cognitive dysfunction, and MRI of neurodegeneration in rodent models offers great potential to develop this burgeoning area of enormous unmet need in society, which is only now being appreciated as a complication of metabolic disorders.
Renal disorders and injury

Chronic kidney disease (CKD) is a common severe complication of diabetes mellitus and autosomal-dominant polycystic kidney disease, the most common human genetic disease. Early damage can progress to severe injury without specific symptoms, stressing the importance of a better understanding of basic mechanisms of kidney injuries to identify new therapeutic targets. CKD is also associated with metabolic bone disease and vascular calcification. We are studying the biology of glomerular epithelial cells (podocytes) and proximal tubular epithelial cells in order to identify mechanisms of kidney injuries and thereby new therapeutic targets. Using well-researched patient datasets/cohorts, we identify and validate biomarkers in blood and urine of patients with CKD that predict poor outcomes such as cardiovascular disease. We are developing a cohort and biobank of samples from patients with glomerulonephritis to allow verification of insights obtained in preclinical models and testing of therapies. We are also involved in the SPOR project, CAN-SOLVE-GN , recently awarded by the CIHR. This will lead to a national registry of primary glomerulonephritis patients with collection of longitudinal clinical information and biospecimens. As many patients with irreversible kidney disease receive transplants, database and biorepository of kidney transplant recipients are being developed in order to identify trajectories that lead to graft rejection as well as preventive and therapeutic approaches to minimize such rejection and improve transplant outcomes.
Bone, muscle and geroscience
Bone and muscle mass loss in older persons are major causes of impaired mobility, loss of autonomy and death from complications. The Integrative Research Group on Bone, Muscle and Geroscience at the RI-MUHC represents cutting-edge biomedical research dedicated to unraveling the complex interplay between bone and muscle health, and the aging process. Our multidisciplinary group brings together experts from diverse fields such as molecular biology, biomechanics, endocrinology, gerontology, and clinical medicine to advance our understanding of the mechanisms underlying musculoskeletal aging and degeneration and the impact that chronic conditions (i.e., cancer, dementia) have on the musculoskeletal system.
One aim is to identify and characterize the molecular signatures associated with age-related changes in bones and muscles as well as the effect of chronic conditions on those tissues. Through the development of innovative therapeutic interventions, including pharmacological agents, gene therapies, nutraceuticals, cell therapies, and regenerative medicine techniques, we also aim to mitigate the impact of aging on bone and muscle health.
Cell signaling

Cell signalling is critical in mediating the physiological effects of hormones as well as the complications that arise from disordered metabolism. We are exploring the fundamental roles of various signalling pathways as well as the role of compartmentalization of such signalling within the cell. We are also studying the roles of disordered intracellular metabolism and the activation of ER stress, unfolded protein responses and proteostasis in mediating complications of metabolic disorders. Innovative approaches for hormone-signalling activity in cells and in vivo (e.g., biosensors) are designed and used to study defects in hormone signalling as well as to generate novel assays for studying drugs efficacies and toxicities.
We are developing biosensors in autophagy and ER stress as surrogates for metabolic and glomerular diseases. Combining our genomic expertise with biosensors to explore the pharmacogenomics of hormone receptors such as those in glucagon-like peptide-1 (GLP-1), we find that polymorphisms in receptors may be expected to alter patient responses to drugs in distinct ways. Because GLP-1 agonists promote beta-cell function and are cardioprotective, signalling signatures (using biosensors) that support or impair these functions are being evaluated for different clinically used GLP-1 agonists.